When 15-year-old Australian boy Kevin was diagnosed with Early T-cell Precursor Acute Lymphoblastic Leukemia (ETP-ALL), a transnational race against death began. As an extremely dangerous subtype of leukemia, ETP-ALL accounts for less than 5% of all acute lymphoblastic leukemia cases, falling into the category of rare diseases. Over 80% of patients exhibit chemotherapy resistance, with a remission rate of only 30%-40% following chemotherapy. For those who relapse, the 5-year survival rate drops below 10%, making it universally recognized as a "tough nut to crack" in the global hematology community.
Local Australian hospitals quickly initiated high-intensity chemotherapy for Kevin, but drug resistance acted like an impenetrable barrier—cancer cells remained unchecked. More critically, a series of life-threatening complications emerged: sudden lower limb paralysis robbed him of mobility, prolonged immunosuppression left him vulnerable to severe infections, including lung infections and skin abscesses, which eventually triggered septic shock. He was rushed to the ICU multiple times.
After nine months of treatment at two top children's hospitals in Australia and Singapore, doctors delivered the devastating news: "We have exhausted all available treatments. His body cannot withstand further therapy. We advise preparing for the worst." At that point, Kevin was bedridden, battling systemic infections, and had lost significant weight—his life was fading away.
Just as the Thomson family sank into despair, a fellow patient who had received treatment in China recommended Beijing Jingdu Children's Hospital, renowned for treating refractory and relapsed pediatric hematological diseases. The hospital had achieved breakthroughs in precision treatment for ETP-ALL, with numerous successful cases.
Clinging to their last hope, they contacted the hospital's hematology expert team through the international department's green channel, launching a cross-hemispheric life-saving mission. On December 21, 2025, Kevin arrived in Beijing via special flight, supported by his parents (still unable to walk normally). His critical condition posed immense challenges for treatment.
Admission assessments revealed a dire state: Kevin had lost 10kg since diagnosis, appearing severely emaciated; his body was covered in infected pustules, some oozing pus; severe oral mucositis left him unable to eat or speak, relying solely on nasal feeding for nutrition; pressure sores from prolonged bed rest worsened due to infection; he also suffered from Escherichia coli sepsis, with a persistent fever above 39°C, unstable heart rate and breathing, and nearly complete immune collapse. Conquering these complications was critical to advancing further treatment—even a minor infection could prove fatal.
Precision in medication is the cornerstone of leukemia treatment. Faced with Kevin's critical condition and ETP-ALL's chemotherapy resistance, the hospital's hematology team knew blind treatment would only exacerbate his fragile state—only precise diagnosis and therapy could offer a chance of survival.
Breaking free from conventional testing limitations, the team employed dual advanced detection methods: in addition to flow cytometry (used in most countries with a precision of 10⁻⁴), they utilized second-generation MRD monitoring and NGS genetic sequencing, boosting precision to 10⁻⁶. This allowed them to accurately detect minimal residual cancer cells, assess their quantity, activity, and drug resistance gene characteristics.
Using this scientific data, the team precisely adjusted the dosage and type of targeted drugs and anti-infective agents—ensuring maximum efficacy against cancer cells while minimizing additional damage from unnecessary medication, laying a solid foundation for subsequent treatment.
To improve success rates and reduce complications, the hospital designed a personalized, multi-faceted treatment plan for Kevin: based on chemotherapy, it combined CAR-T immunotherapy, targeted drugs, and hematopoietic stem cell transplantation (HSCT), forming a comprehensive "chemotherapy-immunotherapy-targeted therapy-transplantation" system to specifically tackle drug-resistant cancer cells.
For the transplant, an innovative triple combination model—"haploidentical stem cells + peripheral blood stem cells + umbilical cord blood"—was adopted to effectively reduce rejection risks. Meanwhile, technologies such as PET-CT and bone marrow flow cytometry (FCM) were used to real-time track cancer cell activity, enabling timely detection of drug resistance and dynamic treatment adjustments.
Results were remarkable: pre-treatment bone marrow blasts accounted for 70% with multiple drug-resistant lesions; after CAR-T therapy, blasts dropped to 0.277% with controlled resistant lesions; 28 days post-transplant, peripheral blood chimerism reached 99.9%, with successful hematopoietic function reconstruction.
The team confirmed that HSCT was the only potential cure for drug-resistant patients like Kevin—and time was of the essence. Each day of delay increased relapse risks. Once Kevin's condition stabilized slightly, the team made a bold decision: abandon conventional CAR-T conditioning (to avoid cytokine storm for his fragile body) and directly initiate HSCT preparations.
Leveraging inter-institutional collaboration, the hospital activated an emergency green channel, quickly coordinating with a radiotherapy facility. Radiotherapy molds were produced within 24 hours, and radiotherapy began smoothly on December 30 to precisely eliminate residual drug-resistant cancer cells. Working around the New Year holiday with seamless departmental coordination, Kevin entered the sterile transplant ward on January 2, 2026—only 12 days after admission. This extraordinary efficiency seized the initiative for his treatment and minimized relapse risks.

A high-quality hematopoietic stem cell donor is critical for successful transplantation. Emergency matching tests identified Kevin's 46-year-old father as the only suitable donor, but advanced age presented a new hurdle: initial stem cell mobilization yielded far less than the required amount for transplantation. Failure to mobilize sufficient cells would mean Kevin losing his only chance of cure.
The medical team abandoned conventional mobilization protocols, using high-efficacy specialized mobilization drugs while arranging autologous blood storage for the father to prevent hypotension, anemia, and other risks during high-volume cell collection. After 3 days of precise adjustments, the second collection yielded fully qualified stem cell quantities with 98% cell viability—successfully overcoming the core challenge of elderly donor mobilization.
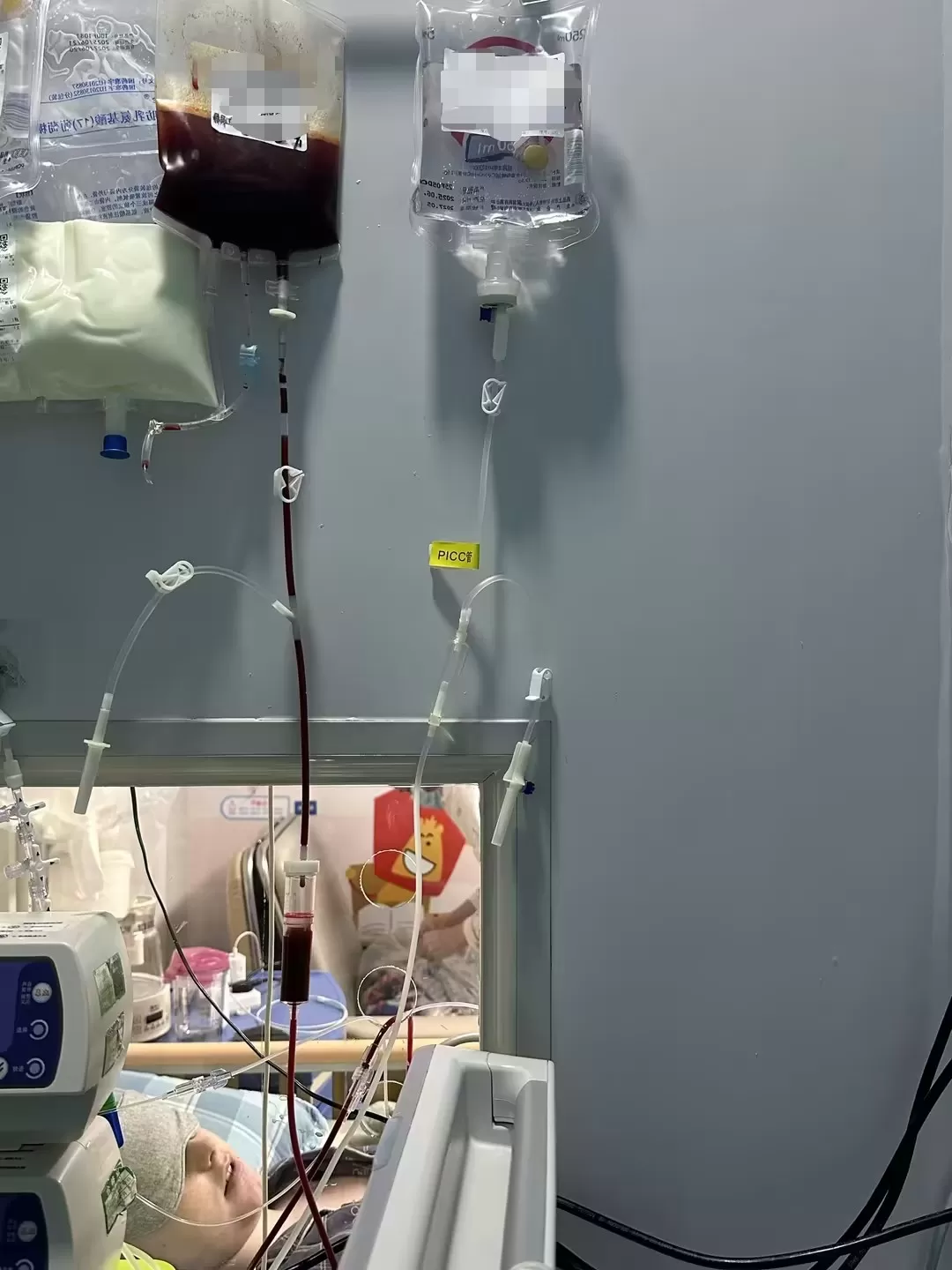
Following Kevin's admission to the transplant ward on January 2, his father's stem cells were transfused smoothly, completing the transplant—but the real test had just begun. Kevin soon entered the period of severe cytopenia, with immunity plummeting. New pustular infections appeared across his body, and his temperature soared to 39.5°C, escalating life-threatening infection risks.
The medical team was well-prepared. Drawing on extensive clinical experience, they closely monitored Kevin's vital signs and infection markers, precisely adjusting anti-infective protocols with targeted antibiotics combined with immune support therapy. Comprehensive care for the skin, oral cavity, and nasal passages prevented infection spread. Thanks to pre-transplant precision conditioning and timely transplantation, Kevin's body responded positively—immunity recovered rapidly, and all infections were fully controlled within 5 days. Skin pustules healed, oral mucositis improved significantly, and he could gradually consume liquid food, successfully navigating the most dangerous post-transplant complication phase.
Unlike conventional ETP-ALL patients who face slow, fragile post-transplant cell engraftment, Kevin's cell growth exceeded all expectations—attributed to his personalized transplant plan. Considering his fragile constitution and chemotherapy resistance, the team optimized pre-transplant conditioning to reduce treatment-related damage. They also precisely adjusted the dosage and infusion rate of hematopoietic stem cells based on the elderly donor's characteristics, creating optimal conditions for engraftment.
The miracle unfolded: while conventional transplants require 15-20 days for cell engraftment, Kevin's bone marrow aspiration on day 10 post-transplant showed successful neutrophil engraftment—far ahead of schedule. On day 12, peripheral blood chimerism testing revealed donor cell occupancy of 99.89%, achieving complete engraftment success! Rapid, high-quality engraftment not only shortened the immunosuppression period but also reduced complications like infections, laying a solid foundation for smooth recovery.
During treatment, Kevin's lower limb paralysis improved gradually with combined care from the rehabilitation and hematology teams: he could sit independently one month post-transplant and walk with crutches two months later. All systemic pustular infections and pressure sores healed, his weight recovered, and the smile of a teenager returned to his face.
When news of Kevin's successful transplant, complete infection control, and impressive engraftment timeline and chimerism data reached the WhatsApp group of his Australian treating team, the entire group erupted in excitement. Doctors sent three consecutive messages: "Unbelievable! This is a medical miracle! Your team’s professionalism and efficiency saved his life!" Medical staff from Melbourne and Singapore also sent congratulations, jointly witnessing this cross-hemispheric life miracle.
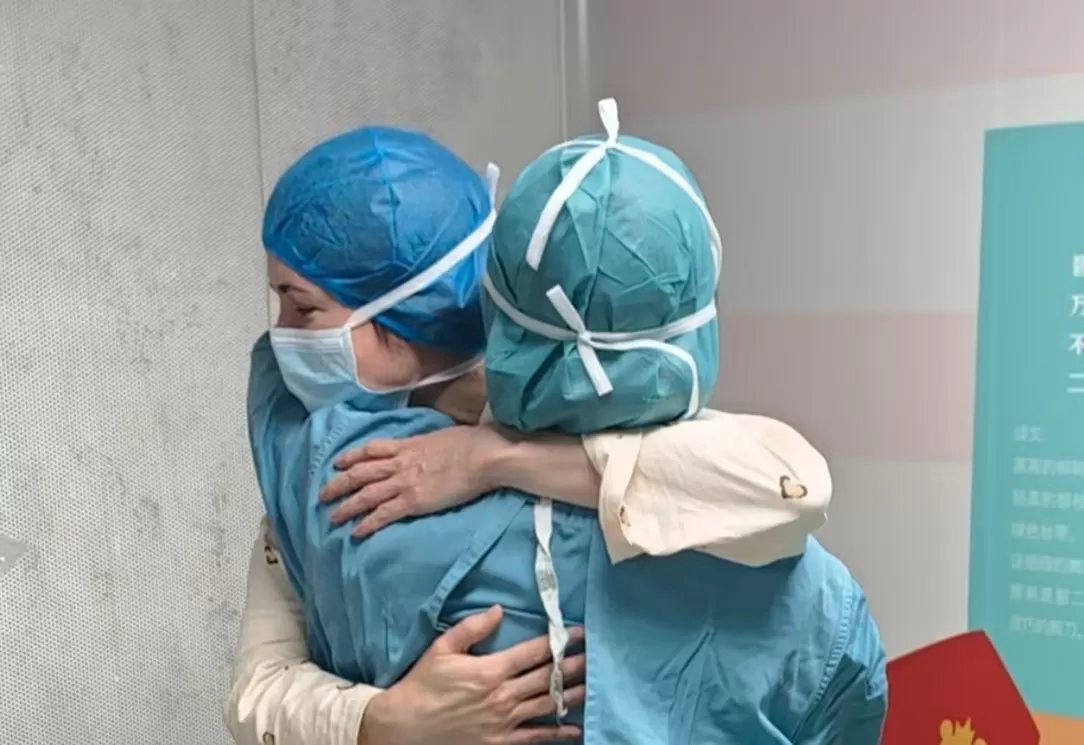
In their thank-you letter, the Thomson family wrote: "We crossed oceans with our paralyzed, dying child to a foreign country. It was the doctors and nurses at Beijing Jingdu Children's Hospital who gave him a second life. You not only cured his illness but also warmed our entire family. This borderless compassion and medical dedication will stay with us forever."
This cross-continental life relay not only restored hope to an Australian family but also showcased China's outstanding achievements in treating refractory and relapsed pediatric hematological diseases. With exquisite medical skills, cutting-edge monitoring technology, personalized treatment plans, decisive decision-making, and compassionate care, the expert team at Beijing Jingdu Children's Hospital overcame one challenge after another. Their data and results prove China's international standing in pediatric leukemia treatment, lighting a beacon of hope for more refractory and relapsed leukemia patients worldwide.